Structural Heart Program
St. Mary's Structural Heart Program started in September 2018 with the launch of Transcatheter Aortic Valve Implantation (TAVI) procedures. In June 2022, our program expanded with the introduction of the Patent Foramen Ovale (PFO) Closure procedure.
The goal of the Structural Heart Program is to use minimally invasive techniques to treat structural heart conditions. Unlike traditional surgery, these procedures do not require opening the chest, and result in shorter hospital stays and faster recoveries for patients.
Structural Heart disease can be present at birth (congenital) or develop with age, and refers to defects in the heart’s valves, wall, or chambers.
Structural Heart Procedures
Our Structural Heart Program offers the following procedures:
- Transcatheter Aortic Valve Implantation (TAVI)
- Patent Foramen Ovale (PFO) Closure
TAVI
St. Mary’s offers a minimally invasive procedure called Transcatheter Aortic Value Implantation (TAVI) for patients with severe symptomatic aortic stenosis.
Aortic stenosis causes narrowing of the aortic valve, which can result in shortness of breath, chest pain, weakness, feeling tired and passing out.
- TAVI is a minimally invasive cardiac procedure to replace aortic valves
- TAVI is intended as an alternative to traditional aortic valve replacement surgery in patients deemed high risk
TAVI is a procedure for patients with severe symptomatic aortic stenosis who are not able to have open heart surgery.
Click here to read the TAVI Patient Booklet, which includes information on things to know beforehand, the risks and the process.
- Print and complete the TAVI Referral Form.
- Referred patients will receive a letter from our TAVI Coordinator to set up a consultation appointment.
- Patients are seen by a team of physicians at the TAVI clinic to assess operative risk and complete further testing if deemed appropriate for TAVI.
- Once accepted, patients will receive a procedure date.
Patent Foramen Ovale (PFO) Closure
What is a PFO?
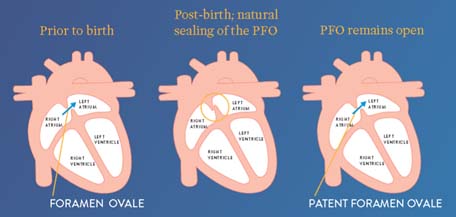
A patent foramen oval (PFO) is an opening in the heart that did not close the way it should after birth. This small tissue flap opening is found between the two upper chambers of the heart, the right and the left atria.
As baby grows in the womb, the foramen ovale allows the blood to bypass baby’s lungs which are not fully developed. Foramen ovale closes six months to a year after baby is born. In about 25% of people, the tissue flap does not close and results in patent (open) foramen ovale. A PFO can allow a small amount of blood to pass from the right to left atria. In some individuals, a PFO may allow a blood clot to pass from right to left side of the heart and from there enter the brain. This results in a stroke or Transient Ischemic Attack (TIA).
During a PFO closure procedure, a doctor inserts the device-tipped catheter into a blood vessel in the groin and guides it into the atrias. Once the catheter crosses the PFO, a small occluding device is deployed, closing the opening. The device will remain permanently implanted in the heart and over time will become covered with heart tissue.
The PFO closure procedure is available for individuals with confirmed PFO who have suffered a stroke or a TIA of unknown origins.
Read more in St. Mary's PFO Patient Information Booklet about the procedure and what to expect.
Contact Rebecca Gies, Regional Cardiac Care Coordinator, TAVI & Structural Heart Programs
519-749-6578 ext. 1992 | Fax: 519-749-6414
- Dr. Tony Wassef
- Dr. Jaffer Syed
Referred patients will receive a phone call from Dr. Wassef’s or Dr. Syed’s office to set up a consultation appointment. Once accepted, patients will receive a package containing booking and procedural information